


EHR implementation is integration of the electronic health records in healthcare workflows. The adoption of EHR software streamlines patient management, enhances communication between different medical professionals, and ultimately enhances patient care quality.
EHR solutions have become an integral part of healthcare providers’ digital mix, partially due to the Meaningful Use program and other government-led incentives for adopting EHR systems, and also because of the software’s vast capabilities. While some organizations swear by their EHRs, others report disappointment and burnout. Multiple factors determine a medical provider’s satisfaction with the system, and successful EHR implementation is one of the major factors.
Table of contents
of European physicians used electronic health records in 2021
of personnel in physician-owned practices are satisfied with their EHR
CAGR of the global clinical EHR market from 2022-2027
Scheme title: Adoption of EHR by hospital service type in the USData source: healthit.gov — Adoption of electronic health records by hospital service type 2019–2021
Large healthcare organizations can implement electronic health records software in two distinct ways. An immediate implementation approach calls for simultaneous system rollout in all the departments. In contrast, an incremental approach means the new EHR will be implemented module by module, with user training and system tweaks performed along the way. Each method has its pros and cons and is suitable for different situations.
Quicker healthcare digitization All departments are involved Improvements seen throughout the organization immediately
Easier to locate and fix any issues before they affect the entire organization Less productivity disruption due to a gradual transition
Requires significant resources from the healthcare organization and time and effort from the medical personnel
Requires close collaboration with the EHR vendors and strict data governance to eliminate the possibility of data loss or contamination during the transition
Based on our experience, regardless of the chosen adoption approach, there are seven key steps providers need to take to overcome common roadblocks and ensure a smooth EHR system implementation.
1 Involve medical specialists 2 Map out the workflows 3 Create a clear EHR implementation plan 4 Ensure usability 5 Migrate data 6 Train your personnel 7 Keep the improvement goingGather a team of healthcare specialists who will collaborate with the development provider’s team members in order to create an EHR tailored to actual clinical workflows and specifics. Clinicians don’t need specific programming skills. They will just monitor the development to ensure the system’s usability and then help mitigate employee resistance to change to facilitate EHR adoption.
Before heading to the EHR adoption process, examine the clinic’s processes and how EHRs can improve them. As a rule, outdated or illogical workflows make top candidates for a redesign. When assessing the workflows clinicians shouldn’t use lengthy and wordy descriptions but instead, go for easy-to-read flowcharts. Workflow mapping usually involves five stages, from setting the start and end points to analyzing the current situation and drafting routes for improvement. The most common measures here involve eliminating redundant steps and reducing delays.
Now that the main points for improvement are visible, stakeholders can create a clear list of requirements for future EHR. The EHR implementation team can use this list as a starting point to calculate the approximate time and budget needed for the deployment. Finding a suitable specialized solution, like a psychiatric or a pediatric EHR, might take longer, while selecting and setting up a general-use out-of-the-box system is faster and easier.
After negotiating with the EHR implementation provider and signing the contract, the project team starts working with them on an implementation plan. The implementation experts can change the implementation process and make it more efficient, proposing additional measures like training and setting up crucial data backups.
Ensure that the focus group consisting of clinicians is involved in the EHR implementation from start to finish, not only during the planning stage. These professionals are more likely to detect flaws and potential issues, from time-consuming digital chores to potentially deadly situations, like incorrect drug dosage due to misspelled units of measurement. During all stages of EHR implementation, clinicians inspect the system and submit their feedback to the development team. After the rollout, the implementation team can assess the system's usability with the help of expert reviews, performance testing, usability metrics, and risk assessment.
Data migration scenarios are varied and plentiful: you can transfer information from paper records to EHR, from an old system to a new one, or from a locally hosted to a cloud-based system. It is a complex process that requires vigilance because low-quality or broken data can affect the accuracy of the clinicians’ decision-making process and further compromise other operations.
Testing and going live
Audit and maintenance
Scheme title: A data migration strategy
The transition to a new system forces medical professionals to change their well-established workflows and adapt to the new technology swiftly. To make the process seamless and reduce the related stress, EHR software providers should lend clinicians a hand with training courses. It’s vital to show the clinical staff the most widely used commands and make sure they are able to execute them. When clinicians get comfortable with the basic EHR functions, they can move on to more complex tasks.
Another important part of the training is security. Personal health information often becomes the target of hacking attacks, which cost healthcare providers billions of dollars. Increasing cybersecurity awareness can help prevent phishing and spoofing that have surged in frequency during 2021, according to BakerHostetler’s 2022 Data Security Incident Response Report.
Scheme title: The correlation between satisfaction with the EHR and agreement that ongoing training is effective
Data source: klasresearch.com — Global EHR Satisfaction 2022
Even after the EHR software has been successfully deployed, its owners can decide to improve the system's productivity, expand its capabilities, or strengthen its security through different types of modifications. For example, making EHRs telemedicine-ready can help combat today’s challenges, like the COVID-19 pandemic. It is also possible to solve some recurring EHR challenges via EHR migration, since a cloud-based EHR can, for instance, spare the owners the worry about the ever-growing volume of patient data to store.
The time and budget needed for a successful EHR implementation depend on many variables: whether it is a proprietary system or an open-source EHR, what feature scope and integrations with EHR it should include, and who the potential users would be. The implementation team usually calculates the approximate EHR costs and implementation timeline for your particular case, but it still can change a bit down the line if unforeseen circumstances arise.
While EHR software offers significant benefits to healthcare providers “as is”, it can simplify even more processes and boost profits if supplemented with integrations relevant to the particular medical practice.
Key integration options Patient portals Telehealth Financial and insurance management systems Lab management systems Hospital management software Healthcare CRMImprove doctor-patient communication and reduce routine tasks for healthcare staff by letting patients view and manage their personal health details and schedule appointments via the patient portal connected to the EHR.
Enable doctors to hold consultations from anywhere and keep the patient documentation synced by letting them upload their examination notes, diagnoses, and treatment prescriptions directly into EHR from the telehealth platform.
Safeguard the financial interactions with patients by allowing only authorized personnel to access their insurance information. Provide patients with flexible payment options that suit their preferences when scheduling appointments.
Reduce lab test waiting time, eliminate errors caused by manual input, and enhance the accuracy of diagnosis and treatment through seamless data flow between a laboratory information system and an EHR.
Distribute tasks and resources among personnel more effectively by uploading appointment scheduling and patient data into the practice management system from the EHR.
Connect your medical CRM with your EHR to improve your sales and marketing efforts and ensure smooth coordination between administrative tasks and clinical examinations, creating a seamless patient care experience.
We support healthcare organizations that adopt EHR for the first time or switch from one system to another by expertly handling each stage of the EHR system implementation.

We help healthcare organizations assess their specific needs, identify main requirements, and outline business and clinical priorities to choose an appropriate EHR system. Our experts also help define a future EHR solution's functionality, usability, interoperability, and cost. We utilize our vast industry expertise to conceptualize a solution that aligns with the organization's workflows and clinical and business objectives.
We ensure the successful implementation of the selected EHR system. This means creating a detailed project plan outlining tasks, timelines, and responsibilities, followed by hardware and software installation, system configuration and customization, end-users’ additional training, workflow redesign, and change management. All relevant information, including electronic medical records and operational data, should at some point be accurately and securely migrated from legacy systems to the new one. Our team streamlines the migration process, enabling seamless patient information exchange and ensuring data accuracy, integrity, and security.
During this stage, the EHR system is integrated into the organization's IT infrastructure and enhanced with various third-party apps, and all relevant data is migrated from legacy systems to the new one. Our team enables seamless patient information exchange and ensures data accuracy, integrity, security, and quality performance of the EHR solution inside the healthcare organization’s ecosystem.
We offer ongoing monitoring and evaluation of the EHR system's operation, adjusting and updating the system if needed to keep its security, usability, and interoperability up to the current quality standards and regulations. We can also provide training sessions to ensure that clinical staff use the system properly and efficiently.
Over the years, we helped medical companies boost their productivity by implementing EHR systems to serve as the primary patient data source.
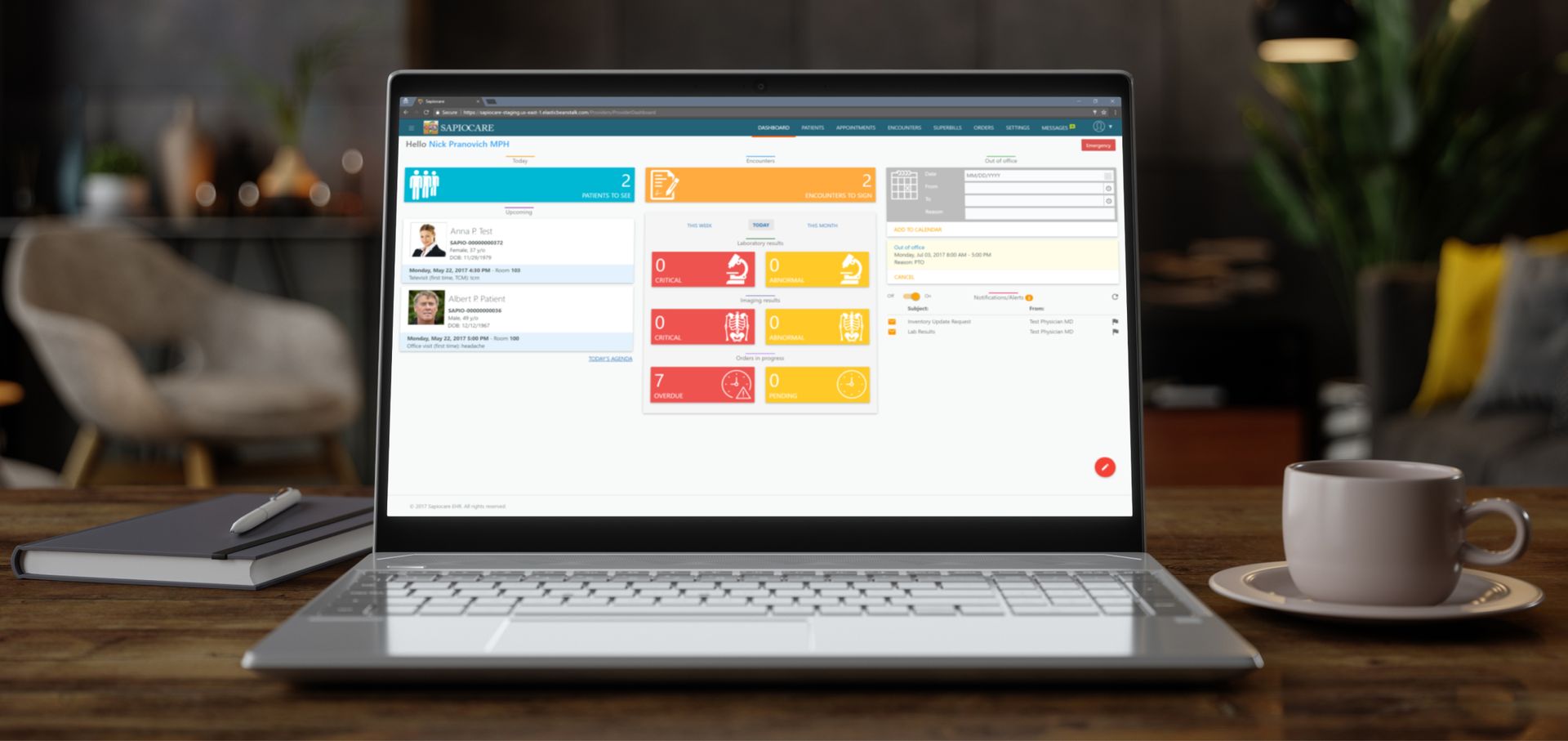
Together with Triptych Technologies Inc., we worked closely with a team of physicians to implement an innovative EHR solution that would support day-to-day clinical operations and simplify decision-making. Secure integrations with other medical service providers like laboratories and pharmacies enabled physicians to access test results or file prescriptions in one place, focus more on patients, and get the most out of the new EHR system while successfully overcoming major implementation risks.

Our team created an asthma monitoring suite as a part of a bigger medical ecosystem. Though our project was mostly about developing mobile apps and the platform for results analysis, we also integrated it with external services and a data exchange channel linked to EHR. The successful implementation of EHR ensured access to patient data for medical personnel, patients, or even analytical software, elevating patient satisfaction.
Despite all the arguments in favor of EHRs, many healthcare providers have valid reasons to be cautious about the adoption of the electronic health record system.
1 Additional workload 2 Сhange management 3 Detachment from patients 4 Poor data governanceMany clinicians believe that dealing with EHRs is one of the major contributors to burnout and cognitive overload.
Pay attention to your clinical team’s feedback during the EHR implementation process to ensure maximum usability of the system. Also, invest in sufficient personnel training so that clinicians use the system effectively.
Too much time spent on bureaucratic tasks
EHR or other IT tools hurt my efficiency
EHR or other IT tools inhibit my ability to deliver quality care
Lack of training/proficiency on EHR or other IT tools
Scheme title: EHR-related contributors to burnoutData source: klasresearch.com — Global EHR Satisfaction 2022
Change is hard, and introducing something new into a company can be met with resistance if not appropriately handled. EHR implementation is more likely to be successful if three phases of productive change management are achieved:
Prepare the ground for change
The organization’s leader should clearly communicate why the change is needed and what the updated workflows will look like for staff, the organization, and the patients. They also need to put together a guiding group of super-users who will drive the change. At this point, the organization’s assets should also be prepared for EHR implementation.
Foster personnel’s buy-in
At this stage, the staff understands how the new system will fit into their everyday operations and what changes they should make to adapt to the new system and workflows. During this phase, the project manager from the healthcare organization’s side must listen carefully to employees and consider the nuances of everyday operations to modify the implementation process if needed.
Implement the change
The change is implemented as a series of steps, during which the system’s operation is reviewed and the arising issues are fixed. The staff learns to handle the new tool, and the guiding group of first users trained and confidently using the system keeps working closely with them to promote change, solve upcoming challenges, or adjust some workflows.
Clinicians are worried about the correct data entry and fewer face-to-face conversations with their patients, which can worsen the quality of care and patient experience. Besides the user-friendly interface and extensive training, AI-supported input tools also simplify data entry. They can be integrated into the medical records software to help clinical staff members focus more on patient care than on working with the system.
A number of EHR systems lack interoperability, so the patient data transfer from one system to another is performed manually, resulting in patient data loss, duplication, inaccuracies, and overall unreliability. Choosing an EHR solution vendor that supports healthcare interoperability would be a step toward the secure flow of data inside the organization. Additionally, regardless of the type of EHR software, every healthcare organization should develop a data governance strategy to ensure its data safety. Such a strategy should be revised and updated each year due to the high volume of healthcare data produced and the variety of possible types of data breach, so it's best to opt for data governance consultants’ services. With expert help, healthcare organizations have more chances to successfully prevent data compromises.